PoTs or Postural Orthostatic Tachycardia Syndrome is a little known syndrome few physicians know about so when young people present at medical offices with anxiety, breathlessness, and rapid heart rate it can sometimes take years before a proper diagnosis is made. Dysautonomia International reports that dysautonomia, an umbrella term used to describe a malfunction in the Autonomic Nervous System, can easily be diagnosed as anxiety or panic disorder.
What is PoTS
PoTs can be caused by anything that places the body under great stress from a virus to giving birth and some are speculating it may be autoimmune.
The definition of PoTs is that while the blood pressure drops, the heart rate rises when one is taken from a lying down position to a standing position and fainting (on occasion) ensues. The heart rate overcompensates the low blood pressure by speeding up, desperately trying to get blood to the brain.
Physicians are just getting a handle on the syndrome and so most sufferers are seen at teaching hospitals such as Stanford, the Mayo Clinic, and other hospitals. However, out of all the specialties in the general physician population, Cardiology is the most up-to-date with the syndrome.
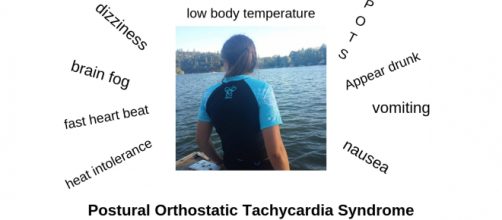
PoTs can present with dizziness, rapid heartbeat, anxiety, panic, nausea, vomiting, diarrhea and/or constipation, chest pain, exercise intolerance, overwhelming exhaustion, and breathing difficulties. Some people have very mild cases of Postural Orthostatic Tachycardia Syndrome while others, up to 25% of people with PoTs Syndrome, are permanently disabled.
There is no cure, but medications help.
How it affected me
In 2018, I landed in the hospital twice with Crohn’s disease, when it was discovered that my blood pressure dropped by 30 or more points systolic upon standing and my diastolic dropped by at least 10 or more points from laying to standing. My heart rate would exceed 160 beats per minute, and I would drop to the floor in a faint. Unbelievably, I could not walk from my hospital bed to the bathroom without losing my breath. I was living in a state of panic and constant anxiety. I had no idea what was happening to me. Just a few weeks before I was in a Crohn's flare, but I could take care of myself. Not anymore.
Along with a horrific flare of Crohn’s disease, I had developed something no one knew anything about.
The doctors tested me for everything they could think of with no answers to my myriad of symptoms. One physician was sure I had adrenal fatigue and soon failure. They knew I had Crohn’s disease, but aside from the rapid heart rate, I also had Orthostatic Hypotension. Meaning that I fainted when I stood up. They gave me yellow socks at the hospital and I was identified as a fall risk. Eventually, the hospital released me on high doses of steroids and referrals to several different doctors who might have answers to my symptoms.
When I got home, I was unable to function. I relied on my family for everything. Just getting off the couch or bed was an effort. I couldn’t even drive a car. Going out of the house continues to be a huge issue for me.
Although my medications help my blood pressure stay up when I eat most of the blood rushes to my stomach leaving me completely drained. On bad days I don’t drive and stick close to home. Everything I do is centered on how I feel each day and sometimes, each hour.
No one thought of PoTs in the beginning because it is something young people develop. I was sent to Stanford where Dr. Sinn put me through a battery of tests that made me very ill. It was decided that I had peripheral neuropathy of the vagus nerve and Postural Orthostatic Tachycardia Syndrome. While peripheral neuropathy of the vagus nerve is listed under dysautonomia it has a far worse outcome. As the physicians keep telling me, it just gets worse, not better.
This is generally said followed by a hug for support.
Peripheral neuropathy causes the small ends of the larger nerve to die. At the moment, those nerves are telling my heart to beat too fast. Eventually, when they die, my heart will beat too slow. And a pacemaker can’t help if the nerves are not there to send the message. I have difficulty speaking. I get hoarse easily and like everything else, some days are better than others. My digestive track is a mess from Crohn’s and peripheral neuropathy has made it worse. If I think about it too much, I get depressed, but the one positive thing I can do is to use my experience to help others. Because I have both conditions, I can reach out to young ones suffering from PoTs to help them better understand how to get help.
Instead of crying, I took my Health into my hands and got off the couch. I joined a gym. The first day after lifting weights (three pounds), I got on the elliptical. When I got off, I was so sick I thought I was dying. The last place I wanted to go was the hospital, so I curled up on the bathroom floor, nauseated, dizzy and just wishing I could die so I didn’t have to go through this anymore. I didn’t die, but I did learn that if you are suffering from dysautonomia it is best to take exercise very slowly.
The same is true for PoTs patients. Exercise is a killer, but it must be done if you want any kind of a life at all. I am now able to lift eight pounds and my stamina has increased. On good days I can drive and I think I’m having more good days than bad, but I have to be careful.
If I overdo I will end up in bed for several days until I recover. I still cannot deal with any kind of stress, but since I started exercising, I drive more often and can walk around a store without stopping to rest. It isn’t much I know, but it’s enough.
Midodrine is my go-to drug for raising my blood pressure while atenolol is my drug of choice to lower my heart rate. It is a balancing act at best because sometimes I have high blood pressure. I supplement with lots of salt, salt tablets actually, and water. Lots and lots of water. I also binge on potato chips and anything salty. It works for a time but has to be repeated daily until I am so sick of salt I want to vomit. I keep my blood pressure machine with me so I can check it.
Sometimes when the exhaustion kicks in it can feel like low blood pressure so before I take the Midodrine I have to take my BP. It has been explained to me that stroke is very common with my condition(s).
The challenge
Worldwide, dysautonomia groups are seeking sufferers to get out there and shout about PoTs syndrome. The best way is through social media. Young people are connecting with other young people about their symptoms and as the conversation grows more and more teens are becoming familiar with dysautonomia.
If you are suffering from anxiety, lightheadedness and/or fainting, nausea, vomiting, rapid heart rate, speak with your parents and loved ones then call your primary doctor for a referral to a cardiologist or to a teaching hospital.
There is help available and if you are not diagnosed with anxiety, PoTs is a treatable syndrome that can change your life. Even if you have PoTs, anxiety is common. Having your heart running at 160 is quite a scary feeling. I did a search to see if I could find television shows featuring PoTs and was excited to find that PoTs was featured on an episode of 'House'.
Recovery
People can recover from Postural Orthostatic Tachycardia Syndrome, but it takes time, in some cases up to five years or more. Treatment includes salt, water, and medication to keep the heart rate down and the blood pressure up. Symptoms can be life altering, but sometimes just knowing what you have is the first step in recovery. While I may never fully recover I am better. I can accept my quality of life because I am older. Being young with PoTs is a far different story, but recovery happens every day.